Common Digestive Disorders
In the intricate dance of health and wellness, the digestive system plays a leading role, often setting the rhythm for our overall well-being. Understanding the nuances of digestive disorders is not just about recognizing symptoms; it’s about tuning into our body’s subtle signals. In this comprehensive guide, we’ll explore 15 common digestive disorders, weaving through symptoms, personal experiences, and expert insights to paint a clear picture of gastroenterology issues.
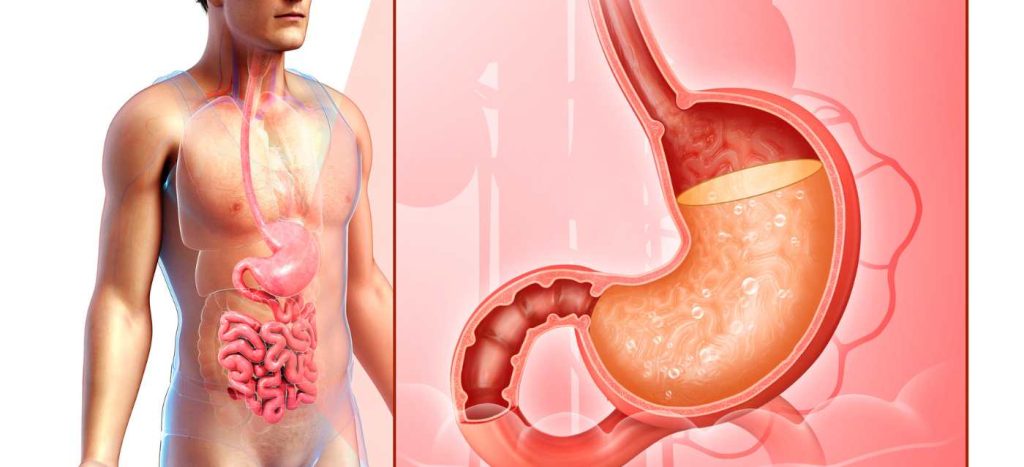
1. Gastroesophageal Reflux Disease (GERD)
Symptoms: Heartburn, acid reflux, chest pain Personal Insight: John, a 45-year-old teacher, thought his chest pain was stress-related, only to discover it was GERD, a condition manageable with lifestyle changes and medication.
2. Irritable Bowel Syndrome (IBS)
Symptoms: Abdominal pain, bloating, diarrhea, or constipation Expert Opinion: Dr. Smith explains, “IBS is often a diagnosis of exclusion. It’s important to rule out other causes before confirming it.”
3. Inflammatory Bowel Disease (IBD)
Symptoms: Chronic diarrhea, abdominal pain, blood in stool Study Findings: Research indicates that IBD, including Crohn’s disease and ulcerative colitis, may have genetic links.
4. Celiac Disease
Symptoms: Bloating, diarrhea, anemia, weight loss Real-Life Example: Emily, diagnosed with celiac disease, found relief by switching to a gluten-free diet.
5. Peptic Ulcers
Symptoms: Stomach pain, nausea, bloating Common Misconception: Contrary to popular belief, stress and spicy food are not direct causes of ulcers but can exacerbate them.
6. Gallstones
Symptoms: Severe abdominal pain, jaundice, fever Expert Insight: “Gallstones can be silent or extremely painful. Regular check-ups are key,” advises Dr. Lee.
7. Lactose Intolerance
Symptoms: Bloating, diarrhea, gas after dairy consumption Personal Tip: Maria shares, “Switching to lactose-free products drastically improved my symptoms.”
8. Gastroenteritis
Symptoms: Vomiting, diarrhea, abdominal cramps Preventive Measure: Good hygiene and proper food handling can prevent many cases.
9. Diverticulitis
Symptoms: Abdominal pain, fever, changes in bowel habits Dietary Advice: A diet high in fiber can help in preventing diverticulitis flare-ups.
10. Constipation
Symptoms: Difficulty in bowel movements, hard stools Lifestyle Adjustment: Increasing water intake and fiber can alleviate symptoms.
11. Pancreatitis
Symptoms: Severe abdominal pain, nausea, vomiting Medical Insight: “Pancreatitis can be acute or chronic and requires immediate medical attention,” notes Dr. Gupta.
12. Hepatitis
Symptoms: Fatigue, jaundice, abdominal pain Awareness Point: Vaccinations and safe practices are crucial in preventing viral hepatitis.
13. Hemorrhoids
Symptoms: Bleeding during bowel movements, itching, discomfort Comforting Advice: Over-the-counter treatments and warm baths can offer relief.
14. Anal Fissures
Symptoms: Pain during bowel movements, blood on stool Healing Approach: Most fissures heal with conservative treatment, like increased fiber intake.
15. Gastroparesis
Symptoms: Vomiting, nausea, feeling full quickly Patient Story: Linda’s diagnosis of gastroparesis led her to modify her eating habits, greatly improving her quality of life.
Gastroenterology Billing Services
For both patients and healthcare providers, navigating the financial landscape of treatments for gastroenterological issues can be as complex as diagnosing the disorders themselves.
Efficient and accurate billing services are essential in ensuring that patients are not burdened by billing errors and that they fully understand their insurance coverage and out-of-pocket responsibilities. For healthcare providers, robust gastroenterology billing systems streamline the process, allowing them to focus more on patient care rather than administrative tasks.
This integration of effective billing practices plays a vital role in the overall healthcare experience, ensuring that the journey towards managing digestive health is not hindered by financial complexities and uncertainties.
As we continue to explore advancements in gastroenterology, the importance of efficient billing services remains a key component in delivering comprehensive and compassionate care.
Preventative Measures for GERD

- Dietary Changes:
- Avoid trigger foods such as spicy, fatty, or acidic foods, and caffeine, which can worsen reflux.
- Reduce the size of meals and avoid eating close to bedtime.
- Weight Management:
- Losing weight if overweight can significantly reduce the pressure on the stomach, thus lessening reflux.
- Elevate the Head During Sleep:
- Elevating the head of the bed by about six to eight inches can help prevent stomach acid from rising during the night.
- Avoid Smoking and Limit Alcohol:
- Smoking can weaken the lower esophageal sphincter and alcohol can trigger reflux symptoms.
- Chewing Gum After Meals:
- Chewing gum can increase saliva production, which may help neutralize stomach acid.
Lifestyle Adjustments for Gastroparesis
- Smaller, More Frequent Meals:
- Eating smaller, more frequent meals can help manage symptoms by reducing the burden on the stomach.
- Softer Foods and Liquid Diet:
- Softer foods and, in more severe cases, a liquid diet can be easier to digest and pass through the stomach.
- Avoid High-Fiber and High-Fat Foods:
- These foods are harder to digest and can slow down gastric emptying.
- Stay Upright After Meals:
- Remaining upright for at least two hours after eating can help gravity assist with digestion.
- Manage Blood Sugar Levels:
- For those with diabetes, managing blood sugar levels is crucial as high blood sugar can slow down digestion
- Read more: Discover the World of Fruitarian Recipes
Dietary Advice for IBD
- Low-Residue Diet:
- A low-residue diet, which is low in fiber, can reduce the frequency and volume of bowel movements, thus easing symptoms during flare-ups.
- Avoid Trigger Foods:
- Common triggers include dairy products, spicy foods, alcohol, and caffeine. It’s important to identify personal triggers.
- Adequate Nutrition:
- Ensuring a balanced intake of nutrients is vital, as IBD can lead to malnutrition. Supplements may be necessary.
- Hydration:
- Adequate fluid intake is important, especially if diarrhea is a frequent symptom.
- Probiotics:
- Some studies suggest that probiotics can help maintain remission and improve symptoms.
It’s important to note that these are general guidelines, and individual responses may vary. Anyone with these conditions should consult with a healthcare provider or a dietitian for personalized advice. Additionally, ongoing medical treatment may also be necessary alongside these lifestyle and dietary changes.
Conclusion
Our journey through the landscape of digestive disorders reminds us of the complex interplay between our body, diet, and lifestyle. While some of these conditions are easily managed with minor adjustments, others require medical intervention. The key takeaway? Listening to our bodies and seeking timely medical advice can make all the difference. As we ponder the future of gastroenterology and digestive health, let’s remember that awareness and proactive care are our most trusted allies in the quest for good health. Remember, in the world of digestive disorders, knowledge is not just power; it’s prevention.